In Fighting Disease Outbreaks like Coronavirus, Don’t Forget About the Health Workers
At the start the Ebola outbreak in 2014, I traveled to West Africa to lead a CRDF Global project on emergency response and preparedness. I walked into an abandoned hospital in the middle of Liberia, where I found two brave nurses delivering a baby. I asked them about the risks they faced, and they replied, “Ebola doesn’t stop babies and the need for us.” It was there that I was first introduced to Maybelline, a delivery nurse who became ill with Ebola as a result of her courageous service. Her husband Moses – with sandals, no gloves, and no personal protective equipment –refused to leave her side. As she prayed, he sang and cooled her down with a wet towel. Maybelline would succumb but Moses survived.
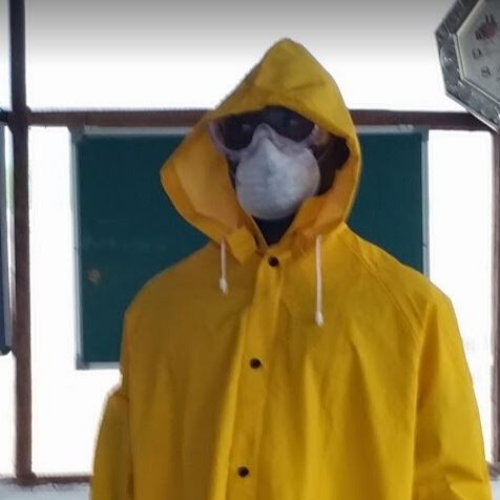
First responders like Maybelline are on the frontlines of emerging infectious diseases. Instead of running away from infectious disease threats, they run towards them. This includes healthcare workers, laboratorians, EMS, first responders, and anyone who serves on the frontlines of emerging infectious diseases. During an infectious disease outbreak, health workers are especially vulnerable to residual risk, which the World Health Organization (WHO) defines as risk that remains after carefully selected control measures are applied. Despite resources and emergency funds meant to keep health workers safe, many lose their lives to the very disease that they are protecting others from. In fact, it is believed that more than 3,000 health workers have already been infected by COVID-19.
While many agencies seek to minimize the health effects of the virus on the general public, there is an opportunity for organizations to better support brave healthcare workers in high-risk situations. We desperately need more innovative programs which monitor their day-to-day health, support their families, address incidents and accidents, and ensure strong safety cultures within the work environment.
How can the global health community better protect health workers?
Sustained global health funding for emerging and known infectious disease threats.Budgets must reflect the emerging reality. Existing threats like influenza, antimicrobial resistance, and healthcare associated illnesses continue to pose challenges to the current technologies available to those fighting infectious diseases. Emerging infectious disease threats lead to measurable losses in the economy and public trust. Sustained public funding from U.S. government agencies like CDC, USAID, Department of Defense, Department of State, and NIH will allow for the adequate stocking of resources, development of new technologies, and continued research on clinical/prophylactic technologies which are necessary to counter emerging and existing infectious disease threats. These efforts also include the use of remote-based technologies and strategies to minimize fear, attack stigmas, and educate the general public on good decision-making during emergency situations.
Develop a biological risk workforce that includes infectious disease first responders, public health agencies, business, and community members. Infectious diseases will always pose a level of inherent risk, which are defined by WHO as risk associated with activities or procedures that are conducted in the absence of mitigation measures or controls. However, many controls have been put in place to minimize the known risks associated with emerging infectious disease threats. But what are the unknowns? These residual risk factors directly deal with human behaviors, psychosocial effects and systematic motivators (social norms), which change quickly as a result of the direct threat of infectious diseases. Though we cannot accurately predict what emerging infectious disease threat is next, we can predict the needs and behavior of those directly impacted by applying lessons from recent outbreaks of Ebola, SARS, MERS, and H1N1.
Utilize technology for protecting against and responding to infectious disease threats.Just like infectious diseases, remote-based training technologies don’t recognize borders. With improved internet access around the world, remote-based technologies can be used to increase awareness, partnerships, skills, and self-efficacy among those responding to infectious disease threats. We should practice techniques and develop procedures before the next infectious disease appears, for it will be a matter of when, not if.
COVID-19 provides a clear signal that more preparation is needed. SARS infected approximately 8,000 in 2013, with a 10% fatality rate. To date, just under 2,500 cases of MERS have been reported with a 34% fatality rate. COVID-19 is already past 70,000 cases, and the mortality rate cannot yet be determined.
Being prepared means building resources, training, partnerships, and public trust. By the time we face a disease with both high transmission and high mortality, it may be too late.
About Sean KaufmanSean Kaufman has led crisis and risk communication and emergency preparedness related to HIV, waterborne disease outbreaks, the anthrax attacks, SARS, West Nile Virus, Monkeypox, H1N1, and Ebola. He is a Certified Health Education Specialist (CHES), Certified in Public Health (CPH), and a Certified Professional in Biorisk Management by the International Federation of Biosafety Associations (IFBA).
Insights posts represent the views of the authors and do not necessarily represent the views of CRDF Global.



